By Ilia Stambler
By Ilia Stambler
The need to develop policies for healthy longevity promotion
The global society is facing the rapid population aging and the accompanying rise of aging-related ill health and the resulting social problems. This mounting challenge stares us all in the face and prompts the global community to seek remedies. At the same time, we also witness the rapid development of biotechnology and medical technology, fostering our hope to find effective therapeutic solutions to the increasing health challenges. The urgency of the problem, and the increasing possibilities for solutions, bring the issues related to population aging and the research, development and utilization of anti-aging, life-extending and healthspan-extending technologies or “longevity therapies” to the forefront of responsible social debate.[1]
Many pressing normative questions arise in this context. What should we do, as a society and as individuals, given the intensifying problems of aging and the possibility and desirability of their solution and as a result achieving a significant healthy longevity extension? How can this possibility be realized? What actions exactly should be taken? Who should undertake those actions? Who should make the decisions about the actions? And who will enjoy the results of those actions? Could there be undesirable side effects to those actions? Such normative questions translate into specific and urgent questions for public health and science policy. For example, should a greater support be given to basic, empirical, applied, engineering, environmental, or other approaches for the amelioration of degenerative aging processes and achieving healthy longevity? What should be the civic regulatory mechanisms of such support? Given the rapid population aging and the increasing incidence and burden of aging-related diseases, on the pessimistic side, and the rapid development of medical technologies, on the optimistic side, these become critical social challenges and vital questions of social responsibility.
Specific regulatory, organizational and policy frameworks will yet need to be developed to address those questions, in any deliberate effort to achieve healthy longevity for the population. It may be yet too early to provide any strictly specific regulatory and policy recommendations toward this achievement. To provide more thorough recommendations, the issue still needs to be raised more strongly in the public, academic and political discourse. Yet, some preliminary recommendations may be offered. These may include increased funding, incentives and institutional support for research and development specifically directed toward alleviation of the aging process and achieving healthy longevity. Some preliminary recommendations are given in the position paper of the International Society on Aging and Disease (ISOAD), entitled “The Critical Need to Promote Research of Aging and Aging-related Diseases to Improve Health and Longevity of the Elderly Population” (2015).[2] Below some of the suggestions of that position paper are quoted and briefly commented on, with specific reference to funding, incentives and institutional support. It must be emphasized that this list and comments are only preliminary, and are intended to stimulate further discussion, encouraging the academic community, the general public and policy makers to elaborate on the present points and add new ones.
According to the ISOAD position paper, “Governments should ensure the creation and implementation of the following policies to promote research into the biology of aging and aging-related diseases, for improving the health of the global elderly population.” The following discussion is organized according to the main policy suggestions and their specific points.
Policy suggestion 1: “Funding: Ensuring a significant increase of governmental and non-governmental funding for goal-directed (translational) research in preventing the degenerative aging processes, and the associated chronic non-communicable diseases and disabilities, and for extending healthy and productive life, during the entire life course.”
Commentary: The importance of increasing funding for biomedical research to increase its produce should be obvious. The soil should be fertile to bear fruit. Yet, sometimes the fruits (longevity therapies) are expected without infrastructure, investment and labor. One often hears from the critics and bystanders of longevity science: “When will we see the results of this research?” or “When will it become relevant to humans?” To which the longevity research advocate can answer: “Right after the research is given more time, care and support.”
Unfortunately, it is often tacitly implied, and sometimes even openly stated, by lay persons and policy makers, that fundamental and translational biological research of aging is somehow wasteful or inherently dangerous, or that the scientists already have ‘more than enough’ and should not ask for more, or that the research money should be better spent on causes other than “aging-related” ill health (as if there are such “aging-unrelated” causes).[3] Likely as a result of such a dismissive attitude, the funding for aging-related issues generally, and biomedical aging research in particular, has been rather scarce in major international and national health and science support frameworks.[4] This attitude should change if the scientific research of aging is to advance and produce positive results. Increasing research funding should become an explicit and emphatic point of advocacy.
Specific point 1: “Dedicating a designated percentage of budget within relevant ministries, such as ministries of health and/or science, particularly in the divisions concerning research and treatment of non-communicable chronic diseases.”
Commentary: Ministries of health and science may seem the natural candidates to provide such funding, but are not the only possible candidates. A thorough search for and outreach to possible providers of funding will be needed. In practical terms, such increases in funding would necessitate painstaking work of research advocates with the relevant decision-makers and stakeholders, also engaging the support of the broader community. In principle, the need to fund medical research of aging should be obvious, so obvious that the relevant agencies (such as the ministries of health and science) simply should make it a part of their policy. Unfortunately, it is very far from being obvious to many in those agencies. In many cases, the relevant decision-makers are simply not aware of the current research and its capabilities. And even if they are aware, there are quite a few obstacles for making the support of aging research a priority within those agencies, especially if it means shifting some other priorities. It is thus the duty and the task of longevity research advocates, first to explain to the relevant decision-makers the need for research support and then continue pushing for the actual achievement of such support.
The advocates would need to determine the agencies from which funding could be allocated to aging research, find out the possible procedural means to achieve these allocations, and establish contacts to negotiate and eventually achieve them. Presently, most aging research institutions are hardly in the position to hire professional lobbyists or materially support advocacy and public education organizations. The scientists are often simply not aware or dismissive of the benefits of targeted advocacy, and if they are aware of those benefits, they seldom have the time or resources to dedicate to advocacy or public education. But somebody has to do this work.
This work should include both “high level advocacy” with professional stakeholders and decision-makers, and at the same time also the work at the “grassroots” levels, convincing the “lay public” about the importance of this research. The arguments for increasing support for aging research should be clear and compelling on the professional level. Yet, professionals in various agencies may have priorities of their own even to pay any attention to the convincing arguments. They may need some encouragement to pay attention “from below,” from the people for whom the new prospective therapies are eventually intended, in order to intensify the research and development for their sake.
Specific point 2: “Dedicating a specific percentage of the profits of commercial pharmacological, biotechnology and medical technology companies to such research and development.”
Commentary: Pharma, biotech and medtech companies may be often reluctant to invest considerable (or any) resources into R&D for the amelioration of degenerative aging processes to extend healthy longevity for the population. There may be several reasons for this reluctance. For one, the companies’ management may be often not familiar enough with the current state of aging research, even to consider involvement. And when some familiarity is gained, the investment into developing biomedical treatments of aging may appear to them too high-risk and too long-term to undertake. Anti-aging and healthspan-improving therapies are preventive by their nature, attempting to postpone chronic age-related diseases before they become debilitating. And evidential predictive diagnosis and preventive medicine may appear “bad business” to many in the management – with returns of profits too uncertain. Seeking costly “silver bullets” against chronic diseases, when they are already devastating and therefore create eager demand, may seem more lucrative for the companies –they are “businesses” after all. (“Evidential” is emphasized here, as quackery may appear to some people profitable under any circumstances. It should also be noted that here the term “anti-aging” is used in the sense of “therapeutic amelioration of aging” and not in the sense of any purely cosmetic contrivances or futile struggle against the passage of time.)
Thus, commonly, as cynical as it may sound, the companies may have little incentive and interest to develop evidence-based preventive anti-aging public health measures. They are not the only ones to blame. People’s readiness to embark on and adhere to preventive health regimens may be quite low (as experience often teaches). And, in fairness, the anti-aging regimens and methodologies may not yet be validated enough to justify compliance. So it would really make little sense, “business” or otherwise, to invest in developing remedies that will likely not work, and that many people would not use even if they worked.
Nonetheless, the feasibility of developing such preventive means does exist. And a considerable proportion of people (probably including ourselves) may indeed be willing to use such means, when they are proven effective, to diminish suffering from aging-related ill health at an early stage. So “the market” does exist for the companies to become interested. Still, they may not be too quick to rush to invest into the related R&D, but would prefer to pick up and capitalize on ready or nearly ready products, after most of the burden of high risk research and development had already been borne by publicly funded institutions. This does not seem a “fair” attitude, in a sense maximizing profit from bad public health, while not willing to strongly contribute to developing solutions against it. There may be no bad intent, but that is what the lack of investments into preventive health entails.
Is there a way to encourage companies to more responsibly “carry the burden” of anti-aging research and development, for the common benefit? A mandatory obligation for biomedical, biotechnological and pharmaceutical companies to invest some portion of their profits to advance biomedical therapeutic aging research could contribute to a solution. It could help to leverage the enormous material, intellectual and logistic resources of the industry for the healing of humanity’s common predicament and for the benefit of all. This would be a kind of a tax on the health industry to facilitate aging-related research and development, either to be performed by the industry itself or in qualified academic, medical and public institutions. The results from such mandatory R&D investment could be partly owned by the companies, and party stipulated to be shared with the public (the exact specifics can be debated and elaborated).
Of course, the terrible specter of “state interference” into “free market” may be raised by such a proposal. Yet, it may be argued that great value may accrue to pharma, biomed and biotech companies from such investment in biomedical aging R&D, as it would allow them: 1) early entrance into a new, untrampled niche; 2) vast potential markets, including early detection and prevention for broad populations; 3) vast demand by the governments and people; 4) fulfilling a social mission; 5) multiple opportunities for developing new products and services, in pharmaceuticals, diagnostics, analytics, early detection, biomedical technology, etc.; 6) providing wellness benefits for the workforce and life insurance companies. The management of some of the health companies may not yet realize those benefits, sticking with the old “silver bullet” quest. The mandatory obligation to dedicate a part of the profits to biomedical aging research and development, may help “initialize” them into the potential benefits of the field, in a sense “lead the horse to the water”.
Some authors have argued that regulatory recognition of “aging as a disease” (a treatable medical condition) would almost automatically induce pharma, biomed and biotech industry to develop treatments against this indication.[5] Such an argument seems to be rather simplistic. Even if recognizing “aging as a disease,” the development of treatments to “cure it” would still require massive investments of resources that the industry may be unwilling to spend for some of the above reasons. Even evidence-based clinical diagnostic criteria for this “disease” are still lacking,[6] and their very formulation would also require massive research that the industry may not be willing to undertake on its own. On the other hand, mandating the investment of a portion of the profits into such R&D, even a small portion (or with a stipulated minimum), would gently encourage them to take interest in the issue.
Of course, if such a proposition were ever to be discussed in the political and public arena, it would require strong advocacy and public involvement, as such a measure would be unlikely to be initiated by the industry itself, or to fit the current common political agendas. In any case, whether the proposition is ever discussed or not, the increased public interest in developing effective anti-aging and healthspan-improving treatments may, nonetheless, influence the pharma, biotech and biomed in a less direct, but perhaps even a more forceful way. Increasing the expectant and intelligent “customers’ base” for effective, safe and affordable preventive aging-ameliorating therapies may leave the industry no choice but to start developing relevant products for them.
Specific point 3: “Establishing relevant research grant programs on a competitive as well as goal-directed basis.”
Commentary: The field of biomedical aging research is a prime example of an emerging and converging scientific and technological field, undergoing rapid growth of capabilities thanks to improved communication and interaction between diverse agencies and entities. It combines “competition” when specific agencies “race” to rapidly achieve the highly advantageous healthspan-improving capabilities, as well as “cooperation” as these capabilities are unlikely to be achieved by any separate research entity alone, but only thanks to mutual catalysis and joining forces with others. This combination has been sometimes termed “coopetition” – comprising “cooperation” and “competition”. If substantial funding is to be provided by governments to the field of biomedical aging research, it should probably be directed in such a way as to strengthen the “coopetition” capabilities, to encourage both the spirit of excellence and achievement as well as mutual aid and support. Such an inclusive approach should involve as many relevant entities as possible, in order to achieve the fastest beneficial results for the widest community as possible.
Encouraging competition between research institutes will be indispensable, for example through open and competitive R&D tenders and calls for proposals. But cooperation should also be encouraged, for example by issuing calls and tenders to form consortia, specifically for the field of biomedical aging research and development. Such calls and consortia are still rather rare. Alongside the traditional consortia of research institutions, there should also be support for the more novel forms of cooperation, such as “crowd-sourcing” – distributing the research and development tasks among many participants, including “citizen scientists”.
While allowing the free competition of ideas, it is also important to understand what we actually want to achieve thanks to the support. Hence, the calls should be goal-directed, with the overarching goal of effective and safe therapeutic intervention into degenerative aging processes and achieving healthy longevity, yet possibly including more specific goals, such as developing evidential clinical diagnostic criteria for degenerative aging, or devising regenerative medicine interventions for age-related tissue degeneration, or designing and testing pharmacological or physical geroprotective medications, or enhancing data-sharing, or improving education in biomedical aging research – altogether furthering the over-arching goal.
Of course, “consortia,” “goal orientation,” “cooperation” and “synergy” should not become synonyms with monopolistic “cartels”. Research and development programs, especially governmental programs, may be too often prone to “cronyism” and “favoritism,” blocking the development of competing alternative ideas. The vital task of developing aging-ameliorating and healthspan-improving therapies should not fall victim to narrow bureaucratic “exceptionalism” and “selectionism”. It is yet unknown which approach may be the most beneficial, fast and effective to achieve the goal of healthy longevity for all. Therefore it appears yet too early to favor any particular approach very strongly. On the other hand, without strong collaborative work to develop specific research approaches and projects, significant advancement may be unlikely. Instead, many entities would each pull resources to themselves, altogether creating teeming chaotic “Brownian” motion, yet without much noticeable gradient of progress. Balanced support of “coopetition” may be needed to encourage both the plurality of ideas and unity of efforts.
The general support for cooperation and competition in biomedical research of aging should also include support for strategic analysis and consultation, to evaluate the promise and judge the evidence of success of various approaches, ideas and efforts, and their combinations. It should also include support for creative education to foster the emergence of new approaches, ideas and efforts, and their combinations.
Specific point 4: “Mandating incremental or factorial increases of such funding.”
Commentary: It is necessary to guarantee continuous increase of support for biomedical aging research. The demand for aging therapies will likely grow with the population aging, and it is important to ensure that the funding for its development is not suddenly stopped, or depleted or redirected, but intensifies in time to supply the growing need. Such a mandated continuous increase could mean, for example, doubling the funding for the field, say, every 2 or 5 years, or negotiating incremental and/or indexed increases of funding at defined periods of time. Such mandated long term increases would, first of all, require the knowledge or establishment of the baseline for such funding. Such a baseline is often absent and needs to be determined for the very first time, at the country and agency levels. Secondly, it would posit the commitment to continued investments in this research and development.
The exact definition of the field for which such funding should be dedicated can be problematic and a subject of active debate. But as a preliminary guiding principle, the funding should be broadly devoted to biomedical research of aging, specifically directed toward therapeutic intervention into degenerative aging processes to prevent aging-related diseases and to increase healthy longevity. And of course, creating such a specific budget item and ensuring its survival and growth, should not detract from funding other important health research and health care issues.
Policy suggestion 2: “Incentives: Developing and adopting legal and regulatory frameworks that give incentives for goal-directed research and development designed to specifically address the development, registration, administration and accessibility of drugs, medical technologies and other therapies that will ameliorate the aging processes and associated diseases and extend healthy life.”
Commentary: Part of the promotion of healthy longevity research could be accomplished not merely by increasing the amounts of financial investments put into the research, but by optimally effective and productive management of the financial investments, combining financial and non-financial rewards for the advancement of the field. This optimization would necessitate the developing and adopting of legal and regulatory frameworks that give incentives for the relevant goal-directed biomedical research and development. Such incentives should accelerate the development, registration, administration and accessibility of drugs, medical technologies and other therapies that will effectively and evidentially ameliorate the aging processes and associated diseases and extend healthy life for the individuals and for the population.
Specific point 1: “Developing criteria for efficacy and safety of geroprotective therapies.”
One of the primary specific requirements to develop the incentives for biomedical aging research would be to establish the criteria for the efficacy and safety of geroprotective (anti-aging) therapies. Such commonly agreed criteria are presently lacking. Yet, they appear to be absolutely necessary in order to set up the goals and define the merits that should be rewarded or incentivized. In other words, we need to incentivize and promote treatments that “wok”. But what are the signs or criteria that the anti-aging treatments “work” or “can work” successfully? These are not yet established, but they need to be.
There has been recently an intensifying discussion among longevity researchers and advocates about the need to recognize the degenerative aging process as a treatable medical condition.[5,6] That would involve recognizing as pathology the systemic aging-related factors that contribute to diseases and frailty. It is assumed that the common recognition of the problem would drive people and resources toward its solution. Yet, it appears that the primary necessary condition for the degenerative aging process to be recognized as a diagnosable and treatable medical condition and therefore an indication for research, development and treatment, is to develop evidence-based diagnostic criteria and definitions for degenerative aging and for the efficacy and safety of potential means against it. Without such scientifically grounded and clinically applicable criteria, the discussions about “treating” or even “curing” degenerative aging will be mere slogans. How can we “treat” or “cure” something that we cannot diagnose?
Interestingly, the clinical definitions of degenerative aging process and the use of drugs and other treatments specifically directed against it, can be fitted, after some reinterpretations, into major existing regulatory and policy frameworks. Thus, WHO’s International Classification of Diseases (ICD-10) currently already includes the category called “senility,” synonymous with “old age” and “senescence” (carrying the code R54).[7] But there are not yet any general symptoms, clinical definitions or test cases of this condition. These may still need to be developed. Furthermore, WHO’s Global Strategy and Action Plan on Ageing and Health (GSAP) – 2016-2020 (November 2015) includes “Strategic objective 5: Improving measurement, monitoring and research on Healthy Ageing,” with a clause “5.1: Agree on ways to measure, analyse, describe and monitor Healthy Ageing” (Section 95), which recognizes the need for such agreed measures.[8] Also major regulatory authorities, such as the US Food and Drug Administration (FDA) and the EU European Medicines Agency (EMA) have struggled for the inclusion of elderly subjects in all clinical trials that may be relevant for them, and are beginning to search for clinically applicable definitions of the aging process and its concomitants. Thus, the EMA has been continuously searching for a consensus definition of age-related “frailty” and for criteria for effective and safe interventions against frailty, as well as for the accurate general assessment of medication needs of older persons.[9] The direction at the US FDA appears to be similar. Here too the need for the inclusion of older subjects in all clinical trials that may be relevant for them and the necessity for devising specific criteria for their diagnostic and therapeutic assessment are recognized,[10] including the assessment of therapeutic interventions against aging-related “multi-morbidity”.[11] Yet, apparently, these needs have not yet been addressed satisfactorily. There is still no mandatory inclusion of elderly subjects in clinical trials, and no agreed criteria for their diagnostic and therapeutic evaluation, either in the EU or the US, or elsewhere.
Massive and profound consultation of scientists, physicians, policy-makers and other stake-holders will yet be required to develop such diagnostic criteria, as a necessary condition for incentivizing and advancing aging-ameliorating therapy. The consultation should encompass as many authoritative forums as possible. For example, in June 2017, the WHO started a consultation on the development of “essential diagnostics” as a necessary companion for the “essential medicines”.[12] It must be realized that both “medicines” and “diagnostics” of degenerative aging are “essential” for global population health. Other authoritative discussion and implementation frameworks may be utilized.
Specific point 2: “Facilitating in silico and animal testing, and ethical safety-enhanced human testing of such therapies.”
Commentary: Integrally related to the issue of devising diagnostic criteria for degenerative aging and for the efficacy and safety of anti-aging and healthspan-extending interventions is the facilitation of various modes of testing of such interventions. Indeed, in order to infer formal general criteria of the “effectiveness” of anti-aging therapy, we need to be able to measure the aging processes, and to find out what effects the various interventions actually produce in each particular case and process, in order to make generalizations.
The testing modes may include in vivo testing, i.e. testing in the living organism, e.g. in model animals, but also human testing falls under this category. Of special importance for anti-aging and healthspan experiments are long-term tests and tests on old animals and elderly human subjects. Further testing modes may comprise in vitro testing, that is, experiments “in glass” or “in a test tube,” i.e. outside the living organism, including cell and tissue experiments, with various techniques such as “lab-on-a-chip”. There is also in situ testing, i.e. in the original condition or place, for example, in the true conditions and place of a biological process (e.g. an in vitro test under conditions identical with or closely approximating a living organism, or an in vivo test under conditions that are the same or very close with the real living environment), that should be also kept in mind, as often inferences are made between biologically irrelevant or incompatible model systems. And yet another critically important form of testing is in silico, that is, using computer modeling of the system behavior, specifically modeling the aging processes and their modifications. Various testing modalities should be advanced simultaneously, feeding back to each other. Unfortunately, each form of testing has its impediments, both scientific and regulatory, that need to be addressed, within ethical bounds.
Thus, among such impediments, in silico testing is not yet commonly practiced in biogerontology. There is often a deficit of cross-talk between the fields of gerontology and bioinformatics, often due to deficit of relevant training of specialists in respective fields, even though the dialogue between these fields is constantly increasing. The various in vitro testing modes often suffer from logistic obstacles in supply, transportation and utilization of test materials, and deficit of appropriate equipment. Animal testing also frequently faces logistic difficulties and deficits of facilities and equipment. In addition, there are often unfavorable public perceptions and regulatory hurdles for animal trials, and not just in relation to anti-aging research. The perceptions and policies may need to improve for the benefit of aging health research. There is also a demand to develop and disseminate the guidelines for the ethical safety-enhanced human testing of anti-aging, life-extending and healthspan-improving therapies. Such authoritative guidelines are currently rather absent. A further set of incentives may need to be conceived to attract test subjects to participate in anti-aging studies, while protecting their safety, privacy and other benefits.
It should be additionally noted that all the forms and modes of testing are skilled-labor-consuming, time-consuming and cost-consuming. Hence, increased funding is a necessary and primary condition to facilitate any form of testing.
Specific point 3: “Deploying and ensuring geroprotective therapies in the status of adjuvant and life-extending therapies.”
Commentary: Drugs and other medical treatments specifically directed against the degenerative aging process are not yet an accepted category in any official pharmacopeia or regulatory registry. Their inclusion in pharmacopeias and registries may be possible after the development of scientifically grounded and commonly accepted clinical definitions of degenerative aging, which are currently absent and need to be devised. Yet, after the necessary consultation and development of diagnostic criteria, such treatments can become recognized as a common part of pharmacopeias and medical regulatory frameworks. In fact, several major regulatory frameworks already have some preliminary conceptual bases for such a recognition, e.g. the recommendation to evaluate drug efficacy specifically for the elderly by the FDA, or the programs to define and treat old-age frailty by the EMA.[9,10] Thus, the development and application of treatments directed against degenerative aging would not require an extraordinary conceptual or administrative leap. Attempts to include specifically anti-aging drugs as common medicines are already under way, with several notable precedents. In the absence of specific regulatory categories for “anti-aging,” they “adopt” existing cognate conceptual frameworks. Such preliminary efforts could be intensified and expanded.
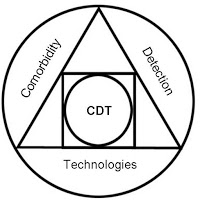
A primary example is the approval by the FDA in 2015 of the clinical testing of Metformin, a well known anti-diabetic drug, as the first drug to treat degenerative aging processes, rather than particular diseases or symptoms. This prospective study was called “TAME” – “Targeting Aging with Metformin”. Such a therapeutic targeting of the underlying aging processes is envisioned as a plausible way to prevent general age-associated multimorbidity, i.e. to postpone the emergence of several age-related diseases and dysfunctions at once.[11] The effects on the basic aging processes would be evaluated by changes in specific biomarkers of aging, while the clinical effects would be estimated by the postponement of clinical signs of several known age-related diseases (multimorbidity), as well as reduced mortality and a reduction of functional decline. There is yet no common agreement on the most informative biomarkers of aging, and no consensus about the evaluation of multimorbidity and functional decline. Still, such a general evaluation and intervention framework – combining putative biomarkers of aging, recognized clinical age-related disease symptoms and syndromes, and demonstrable functional abilities – seems to provide a fruitful direction to follow and develop. Such and similar general combined evaluation and intervention frameworks could be easily understood and adopted both by biologists and physicians. Even though, as of this writing in 2017, funding for this specific large-scope study has not been secured, the study concept may be seminal.
Another example also stems from 2015, when the FDA approved an adjuvant therapy (the adjuvant MF59, made with squalene oil, developed by Novartis) for a flu vaccine to boost immune response in older persons. This development goes beyond “a drug against a disease” model, but seeks an appropriate regulatory framework to support the underlying health of older persons, using “adjuvant” (i.e. “supportive” or “additional”) therapy.[13]
Another approach to develop and advance anti-aging and healthspan and lifespan-extending therapies may be by adopting the concepts of “life-saving therapies” and “life-extending therapies,” that are already well established in major regulatory environments, mainly in relation to life-threatening conditions.[14] Logically, the lifespan-extending therapies are indeed “life-extending” and “life-saving.”
The adoption of the existing regulatory frameworks and concepts, such as “age-related multimorbidity,” “old-age frailty” and “functional decline” to describe the indication, and “adjuvant therapy,” “life-extending therapy” and “prevention of frailty and functional decline” to describe the intervention, may be more acceptable psychologically and better grounded in existing policy than speaking about diagnosis and treatment of “aging” itself. Such an adoption of existing frameworks may be so far the most productive and fast way to develop, test and disseminate anti-aging and healthspan-improving therapies. But eventually it may yet be possible to develop and adopt clinical diagnosis and therapeutic interventions specifically for “degenerative aging” proper, provided the necessary clinical evaluation, efficacy and safety criteria. The development and adoption of such criteria will yet require considerable time, intellectual efforts and material resources. Still, we can state the eventual goal of these efforts clearly and emphatically, without hiding, equivocating or circumventing: we do wish to develop evidence-based, safe, effective and available diagnosis and treatment for degenerative aging to increase healthy lifespan.
Specific point 4: “Providing a shortened approval pathway for therapies with high level of efficacy evidence in preclinical and early clinical trials, as well as in cases of advanced degenerative and seemingly futile conditions.”
Commentary: There is a special need to give priority to the clinical trials and applications of therapies that had provided excellent evidence for their efficacy and safety in preclinical and early clinical trials. Such a prioritizing and fast-tracking of well-evidenced approaches may help bring effective life-saving therapies and improve the quality of life for as many people as possible, as fast as possible. This requirement for good evidence may hold true for any therapies generally, and for anti-aging and healthspan-improving therapies in particular. Yet, regarding the latter, the question remains what constitutes “evidence” of efficacy and safety for anti-aging and healthspan-improving interventions, when there is yet no formal and agreed clinical definition of aging and of its modification. Hence, the need to prioritize the best evidence-based treatments goes hand in hand with the need to develop criteria to evaluate the evidence. Together these tasks may represent critical strategic areas for scientific and policy research.
The clinical approval and application may also need to be facilitated for cases of advanced degenerative and seemingly futile conditions. It seems ethically justifiable to give people a preferential chance of healing when all other hope is taken from them. But here again, there is the problem of the deficit of consensus criteria for defining “enhanced efficacy and safety,” as well as criteria for “advanced degeneration” and “seemingly futile” conditions. For the “seemingly futile conditions,” apparently, the criteria, methodology and terminology from critical and intensive care medicine may need to be reexamined.[15] The existing legal frameworks governing the conditions whose treatment is considered “futile” may be reconsidered in order to allow for the use of novel, less well-tested therapies in severe cases, to give the patients, and potentially others suffering from the same conditions, an improved chance to “live with dignity” rather than to “die with dignity.” Such preferential administration may be advocated for any potentially life-saving and disability-eliminating therapy for the elderly.
Yet, with regard to anti-aging and healthspan-improving therapies, additional complications may arise. In a sense, presently degenerative aging is a universal, inevitable human condition, hence interventions into it may appear generally “futile” for every person on earth. Then when does the futility become “seeming,” i.e. under which conditions some amelioration is possible? The priority treatment of “advanced degeneration” is also not unproblematic. On the one hand, such treatments may be more ethically justifiable, as they would give the patients in this state a unique hope. Any possible clinical benefits in such a state may be most desirable and significant. On the other, it may be very difficult to produce and show clinical benefits in such frail subjects, when the diseases are already highly complicated and hardly tractable (this is often the tacit and rather cynical reason why such subjects are frequently and unjustifiably excluded from clinical trials). Moreover, in principle, anti-aging and healthspan-improving therapies are supposed to be “preventive” – precisely in order to postpone the emergence of such advanced degeneration. Hence intervention at a younger age should be preferable as a preventive measure. The younger subjects may also show stronger responses to therapy (any therapy). But in the case of testing anti-aging therapies in the younger and healthier subjects, there may be little evidence that the intervention will actually produce any benefits for the old age (the presumably desirable outcome). These are complex scientific issues that will yet require a long and resourceful investigation.
One of the more immediate suggestions may be once again to intensify the development of clinical criteria to evaluate degenerative aging, including the evaluation of degrees of “degeneration” and “futility of interventions” – for example, measuring resources available for recovery, or potential resilience, or stability and the speed of return to baseline, or the organism’s complexity, or homeostatic capacity, or others.[16] Such advanced scientific measures of degenerative aging may help gauge and prioritize the therapies, and will help inform further policy and ethical discussion.
Specific point 5: “Granting a special recognition, status and benefits to commercial and public entities engaged in such research and development.”
Commentary: A clear distinction between means of support for public and commercial entities involved in biomedical aging R&D should be made. Public entities should receive substantial tokens of appreciation and support, both symbolic and material, both from the state and from the public, for doing this important research and development. Such support should stimulate them to continue on their path, not let them starve or feel abandoned, not allow the adverse living conditions and lack of status force them to relinquish their scientific and humanitarian mission. The credit they earned and the effort they made should not be taken from them, but should be rewarded.
But what benefits should be provided to commercial organizations to encourage them to enter and remain in the field? After all, as commercial organizations their primary purpose is to make profits, to pay employees their salaries, to produce valuable products and services, to continue and expand the operations. How may it be possible to make it more worth their while to engage in the subject of biomedical aging research and development, in order for them to produce an even greater value for the entire population’s health? The issue is involved. Benefits for commercial organizations have been often understood to include less regulation and less taxation. It has been a commonly voiced opinion that in order to accelerate biomedical progress generally, and the progress of anti-aging and healthspan and life-extending therapies in particular, regulation on the development and use of such therapies should be generally softened, to allow for the proliferation of new ideas and methods.[17] The concept of “conditional approval” of therapies has been advanced, that would presumably make it easier for new therapies to enter the market and would reserve a greater share of research for the “post-market analysis” (i.e. after the medicines have already been sold and used).[18] A considerable number of patients, mainly the wealthy ones, now seek to try new therapies in countries with particularly permissive regulatory requirements, as a form of “medical tourism.”[19] Moreover, personal (“do-it-yourself”) testing is becoming increasingly popular.[20] These customer bases demand more permissive regulation. Thus, diminished regulation is supposed to help health companies to flourish and increase delivery of health products and services, including healthy longevity products and services.
There may be some logic in the argument for easy regulation. The developing and making available of new therapies has become notoriously costly and lengthy, in a considerable measure due to regulatory obstacles, among other reasons.[21] And in many cases, there is a need to try for a chance. On the other hand, we may not wish people (including ourselves) to assume the role of mishandled guinea pigs. Some patients may become privileged gullible test subjects for their own money (if they have money). And others may become expendable unprotected test subjects (when they have no money). Both situations appear ethnically undesirable and may involve a considerable and unjustified risk to the patients’ health and well-being, though possibly with a good “profit margin” and “development potential” for the producers and suppliers of the new medications. Some balanced position needs to be found. Part of the answer may again lie in the development of strict scientific criteria for the diagnosis of the aging process and for the effectiveness and safety of interventions against it. Following the development of such evidence-based criteria, it may be easier to stall the dissemination of quack nostrums as well as to facilitate the availability of truly promising therapies. In other words, such criteria may help improve regulation, not discard it. This issue too should become a subject of broad academic and political discussion.
What about taxation? In a “market-oriented” view, less taxation for companies means more investments, innovation and growth. In a more “social-safety-net-oriented” view, less taxation could also mean larger bonuses for companies’ high management, not necessarily related to better products and services, but with a reduction of social benefits. Could these views be reconciled for the particular benefit of rapid development and universal application of longevity therapies? In an earlier commentary, it was suggested to consider obliging (taxing) health companies to support biomedical aging research. Could it be possible to both reduce taxes for health companies that already develop longevity therapies to encourage their continued R&D in the area, and tax those that do not yet conduct such R&D to encourage them to start? In any case, with a proper balanced consideration of the interests of all the stakeholders, taxation could become a powerful incentive to facilitate the research, development and application of healthspan-improving therapies.
Additional recognition tokens, status improvements and material benefits to encourage the entities involved in the field can and should be thought of.
Specific point 6: “Ensuring affordability of aging-ameliorating and life and healthspan-extending therapies.”
Commentary: Another issue that apparently needs to be given much thought in advance is a normative procedure to make potential anti-aging and lifespan and healthspan-extending therapies universally accessible, rather than preferentially available only to the rich or to some other privileged social categories (unrelated to their medical indications). There may be several approaches to the issue of affordability. Some believe the issue will dissolve almost automatically by itself, as the healthspan-extending technologies and treatments will gradually become cheaper thanks to advancements of the underlying science and enhancing production capabilities. The means of production that could lead to cheaper prices could involve mass production and cheaper customized production, including “do-it-yourself” manufacturing. This scenario may be plausible. The question is: “When will this happen and for whom?” In other words, “How fast can the healthspan and lifespan-extending technologies become affordable enough to become universally available to all?” Until this happens, large masses of people will likely be left out of reach of these therapies. This would mean early death and suffering from aging-related ill health for the largest part of the world population for a foreseeable time in the future, while a small portion enjoys the extended health and lifespan. It has been sometimes argued that the inability to provide longevity therapies to all people (mainly implying the poor ones) should not prevent providing them to some people (implicitly the rich and powerful).[22] Yet, such an argument may offer little consolation to people of lesser means doomed to an early death by their social status, even when proven longevity therapies already exist. (Many readers of this work, and the author, may well find themselves in this group, if no special action is taken.) Such an inequality in healthcare is of course not new. But with the emergence of effective, yet likely initially highly costly lifespan and healthspan-extending therapies, the social divides may become atrocious.
Under such conditions, at least for the initial stages of therapy development, the following options may be available for people of lesser means to make the therapies accessible for them: 1) Wait patiently until the therapies will ‘become cheaper’ and/or ‘trickle down’ from the rich; 2) Fight for the right of access (perhaps also violently); 3) Through advocacy and political action, ensure the establishment of universal public research, development and distribution programs for life-extending and health-extending therapies, that will also give the public strong entitlement to such therapies.
The third option of strengthening public R&D and distribution programs appears preferable, as it would place a large degree of power for the development and application of healthy longevity therapies in the hands of the general public, who are not necessarily related to the scientific, medical or industrial establishment. The first option of resting and waiting until the therapies “trickle down” from the rich may not be very productive (especially if there is no real incentive for the wealthy to provide such therapies to the poor, and also remembering that the decades-long efforts to beg donations for longevity research from the rich have been largely unsuccessful). The second option of “fighting for the right” (of access) may be rather unpleasant, painful and even dangerous for many. Therefore, the third option, establishing programs of public support for therapy research and development, coupled with public entitlement to those therapies, should be more strongly considered and advanced, also by political means.
In any case, the concern over affordability and unequal access should not stop the emergence of new healthspan and lifespan-extending medical technologies, but only to intensify their development. The sooner they emerge, the faster they will likely become available for the people, hopefully for all. Yet, addressing the issue of affordability and accessibility is critical for maximizing public benefits from longevity therapies, and avoiding possible social disruption as their potential side effect. Hence, any effort to develop such therapies should proactively and consciously include plans and provisions to make them maximally affordable and accessible, both through scientific and technological cost-saving contrivances as well as improving the means of equitable social support and distribution.
Policy suggestion 3. “Institutions: Establishing and expanding national and international coordination and consultation structures, programs and institutions to steer promotion of research, development and education on the biology of aging and associated diseases and the development of clinical guidelines to modulate the aging processes and associated aging-related diseases and to extend the healthy and productive lifespan for the population.”
Commentary: In any discussion of healthcare research and development, necessarily involving funding and regulation, aging-ameliorating and healthspan and lifespan-extending therapies must be included as an integral part. Enhanced support needs to be granted to the entities engaged in therapeutic aging and longevity research and development, on a par with any other branch of innovative biomedical science, or perhaps even higher due to the great importance and promise of the field. This essentially means strengthening the institutional basis of aging and longevity science, in all of its aspects, from fundamental science, through translation to clinical practice, to distribution of the results, to public education on the use of the results. And this simply means that we need to have more institutions explicitly dedicated to these subjects, and stronger agendas on these subjects in already existing institutions – on all levels, from small local organizations, to large associations and corporations, to state-level institutions and ministries, to supra-national and inter-national agencies and organizations. Such institutional support is yet insufficient and must be expanded.
Specific point 1: “Establishing Biogerontology specialty and courses in Biogerontology as a common part of university curriculum.”
Commentary: As a part of the stronger institutional support, aging research also needs a better place in academia and other educational frameworks. Good education may be considered a primary condition for progress. There is a need to address the large deficit of knowledge and training on the subject of biological aging, its biomedical improvement and healthy longevity, in most existing institutions of learning. The need should be obvious. It should be clear that prior to any research, development and application on biological aging, there is a need to educate specialists who will be able to contribute to the various aspects of the field. There is an even prior need to educate the broader public on the importance of such research to prepare the ground for further involvement.
Such education is currently very limited. In practical terms, there are presently rather few dedicated structures around the world to promote and coordinate knowledge exchange and dissemination on biological aging and healthy longevity extension. There is an urgent necessity for such structures to make the narrative on biology of aging and healthy longevity globally prevalent.
Dissemination of knowledge in various national languages may be particularly important, as it could dramatically expand global academic and public involvement and cooperation in the field. Indeed, many disconnected chunks of knowledge on aging and longevity extension are scattered around the world. There is much information in various national languages which is not always easily accessible to speakers of English. Conversely, much information is available only in English, while it also needs to be made accessible in other languages. Hence, cross-fertilization of information in different languages could help the entire field to expand globally.
Even in particular languages, the field could benefit from better knowledge communication and data-sharing, specifically within the field of aging and longevity studies, as well as with adjacent fields. It may be argued that virtually any field of science and technology can be related to the problem of aging, and enlisted for its amelioration. Hence the stronger inclusion of biomedical research of aging into the general scientific communication and education could be beneficial for the field of aging, as well as for the allied fields.
To improve the communication and integration, it appears to be crucially important to commonly include biogerontology (or biology of aging and longevity) as one of the central parts of learning curricula, and not only in universities, but in every learning and teaching framework, especially those related to biology, medicine or natural sciences generally. Unfortunately, and strangely enough, the study of the biology of aging and longevity extension is rarely a part of university curriculum and virtually never a part of high school or community education curriculum. Thus, there is a huge range of opportunities to develop educational and training materials and courses, including materials and courses of professional interest, from undergraduate to postgraduate levels, as well as of general interest, presenting recent advances in aging and longevity science. There is a special need for developing courses and other educational materials in national languages, beside English, and in countries and areas in which information on the field is particularly scarce.
Unfortunately, these desires are yet far from fulfillment. The current curricula in life and health sciences around the world, very often, simply omit aging and longevity from processes of biological development. Furthermore, many biology textbooks do not include aging and dying, not to mention longevity, among the processes of life. The science of aging and longevity, and adjacent areas of study, need to become an entrenched part of education at every level, not just because of the scientific value of this subject, but also because of its great practical significance for the society. In fact, the World Health Organization’s Global Strategy and Action Plan on Ageing and Health (GSAP) (2015) directly requests member states to “ensure competencies on ageing and health are included in the curricula of all health professionals.”[23] Of course, it should be stressed that knowledge of the biology of aging is one of such indispensable gerontological competencies. Yet, this requirement is very far from implementation, even as relates to “competencies on ageing” generally, not to mention biology of aging. There is an urgent need to address the problem, to strengthen the standing of biogerontology in academia and other educational frameworks, to cultivate the ground of knowledge necessary for aging research, development and treatment to grow and bear fruit.
Specific point 2: “Developing and disseminating geroprotective regimens, based on the best available evidence, as part of authoritative health recommendations.”
Commentary: Part of the knowledge dissemination and exchange should include actionable recommendations for ordinary people to achieve healthy longevity. It is indeed important to disseminate and popularize the knowledge of fundamental research and its long-term goals. But some more immediate practical outcomes could greatly benefit the public and increase general interest in the field, though never losing sight of the need for long-term fundamental biomedical research and development. The researchers of aging and longevity need to have a say in the development and dissemination of regimens for the extension of healthy longevity for the community, based on the best available evidence, as a part of authoritative health recommendations. Such guidelines for healthy longevity for the public are commonly lacking. There are some examples of limited materials of this kind from major research institutions.[24] But generally such educational activity can be greatly expanded globally.
Specific point 3: “Establishing cooperative centers of excellence for fundamental, translational and applied studies, alongside centers for strategic analysis, forecast, education and policy development on aging and longevity research, at academic institutes and various governmental and supra-governmental agencies.”
Commentary: This is probably the most important and desirable policy recommendation that can be currently made. In fact, it encompasses and engages most of the other recommendations, including increased funding, incentives and institutional support for the field. Simply put, researchers of aging and longevity need places to do their work at. Such work places, that would be involved primarily and not tangentially with biomedical aging research, are quite few even in the “developed” world, and are almost absent in the “developing” or “low income” world.[25] There is a vital need to establish more and more cooperative centers of excellence of different kinds: for fundamental, translational and applied studies. Beside scientific research and development centers proper, there is also a need for supportive intellectual infrastructure, including centers for strategic analysis, forecast, education and policy development on aging and longevity research. Such centers, or at least dedicated thought and task forces, could be desired for virtually all large academic institutes, as the subject has critical academic and public value. Such centers and/or task forces and/or organizational structures should also be present in various governmental and supra-governmental agencies, including virtually all the agencies related to public health and science, but also possible additional entities, such as those dealing with education, social services, or aging generally.
Though the relevance of the topic of biomedical aging research, development and application should be obvious for such agencies and institutions, they still seldom have this subject on their agenda and often not at all. A strong dedicated effort still has to be made to place the subject on the agenda of those organizations. There may be many agencies that may be approached to establish such centers and structures, and the means of approaching and influencing them should yet be studied and perfected.
Conclusion: Normative discussions and recommendations should grow into actions
As a general conclusion, the common rationale for all these tentative policy recommendations is to reduce the burden of the aging process on the economy and to alleviate the suffering of the aged and the grief of their loved ones. It may be hoped that, if granted sufficient support, these measures can improve the healthy longevity for the elderly, extend their period of productivity and their interaction with society, and enhance their sense of enjoyment, purpose, equality and valuation of life. In the light of the great need and promise of healthy human longevity, it may be considered the societal duty, especially of the professionals in biology, medicine, health care, economy and socio-political organizations to strongly recommend greater funding, incentives and institutional support for research and development dealing with the understanding of mechanisms of human biological aging and translating these insights into effective, safe, affordable and universally available life-extending and healthspan-extending technologies and treatments.
We can return to the question asked at the beginning of this work: “What should be normatively done to promote longevity science and the actual achievement of healthy longevity for the population?” Given the feasibility and desirability of healthy human longevity, the normative “thing to do” would be simply “to do,” to become proactive for the advancement of the field, to study and support the field, to realize the challenges facing the field, as well as its vital promises, and to contribute to overcoming the challenges and fulfilling the promises. It may be hoped that the present work will contribute to the realization of this duty. It may be further hoped that the suggestions and comments made in this work will stimulate more consultations to help find solutions for some of the literally “life-and-death” scientific and policy questions of the aging society, to achieve healthy longevity for all.
References and notes
[1] Michael J. Rae, Robert N. Butler, Judith Campisi, Aubrey D.N.J. de Grey, Caleb E. Finch, Michael Gough, George M. Martin, Jan Vijg, Kevin M. Perrott, Barbara J. Logan, “The demographic and biomedical case for late-life interventions in aging,” Science Translational Medicine, 2, 40cm21, 2010, http://stm.sciencemag.org/content/2/40/40cm21.full;
Luigi Fontana, Brian K. Kennedy, Valter D. Longo, Douglas Seals, Simon Melov, “Medical research: treat ageing,” Nature, 511(7510), 405-407, 2014, http://www.nature.com/news/medical-research-treat-ageing-1.15585;
Dana P. Goldman, David M. Cutler, John W. Rowe, Pierre-Carl Michaud, Jeffrey Sullivan, Jay S. Olshansky, Desi Peneva, “Substantial health and economic returns from delayed aging may warrant a new focus for medical research,” Health Affairs, 32(10), 1698-1705, 2013, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3938188/;
Ilia Stambler, “Recognizing degenerative aging as a treatable medical condition: methodology and policy,” Aging and Disease, 8(5), 2017, http://www.aginganddisease.org/EN/10.14336/AD.2017.0130;
Ilia Stambler, “Human life extension: opportunities, challenges, and implications for public health policy,” in: Alexander Vaiserman (Ed.), Anti-aging Drugs: From Basic Research to Clinical Practice, Royal Society of Chemistry, London, 2017, pp. 535-564.
[2]. Kunlin Jin, James W. Simpkins, Xunming Ji, Miriam Leis, Ilia Stambler, “The critical need to promote research of aging and aging-related diseases to improve health and longevity of the elderly population,” Aging and Disease, 6, 1-5, 2015, http://www.aginganddisease.org/EN/10.14336/AD.2014.1210.
Thanks to the translations by longevity research activists from around the world, the text of this position paper became available in full or in part in 12 languages. It is available in full in Arabic, Chinese, English, German, Hebrew, Italian, Portuguese, Russian, Spanish, and as a partial (summary) translation in Danish, Finnish, Swedish. See: http://www.longevityforall.org/the-critical-need-to-promote-research-of-aging-around-the-world/. As of June 2017, this paper was quoted over 40 times in academic literature.
[3] Below are some examples of the works openly disparaging of anti-aging and pro-longevity research, including works by influential state health policy and bioethics advisors and officials, in particular in the US:
Leon Kass, “L’Chaim and Its Limits: Why Not Immortality?” First Things, 113, 17-24, May 2001;
Daniel Callahan, What Price Better Health? Hazards of the Research Imperative, University of California Press, Berkeley, 2003, Ch. 3. “Is research a moral obligation? The war against death,” pp. 64-66;
Koïchiro Matsuura, “Of sheep and men,” The Daily Star, 4 (113), September 16, 2003;
Francis Fukuyama, Our Posthuman Future. Consequences of the Biotechnological Revolution, Picador, New York, 2002, Ch. 4. “The prolongation of life,” pp. 57-71;
Ezekiel J. Emanuel, “Why I hope to die at 75,” The Atlantic, October 2014.
[4]. Indicatively, as of 2016, the entire proposed budget for the Word Health Organization’s “Ageing and Health” program was $13.5M, out of about $4.4 billion total WHO budget (0.3%). No budget portion is specified for anything indicative of “ageing research.”
(World Health Organization, Sixty-Eighth World Health Assembly: Proposed Programme Budget 2016-2017, 2015, http://apps.who.int/gb/ebwha/pdf_files/WHA68/A68_7-en.pdf.)
For the United States (so far the world’s largest spender on health, including aging-related issues), the investments to solve the aging challenge generally and for medical aging research particularly are rather small, despite the urgency of the problem.
Thus, in the US, as of 2014, it was estimated that the total national health expenditures were ~$3.0 trillion, representing 17.5% of the Gross Domestic Product, with yearly per capita health expenditures of $9,523. In 2015, these values respectively grew to 3.2 trillion, 17.8%, and $9,990. All these values are world records. (All the websites quoted here were accessed in June 2017.)
(US National Center for Health Statistics, CDC Centers for Disease Control and Prevention, “Health Expenditures” (2014), https://www.cdc.gov/nchs/fastats/health-expenditures.htm;
US Centers for Medicare and Medicaid Services, “National Health Expenditure Data” (2015)
https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nhe-fact-sheet.html.)
These “health expenditures” should perhaps be better designated as “sickness expenditures” – in a great measure due to the rising aging-related ill health. Yet, the expenditures on biomedical research of aging, to find clinically effective and cost-effective means to curb the aging plague are comparatively miniscule.
Thus, as of 2016, the budget of the US National Institutes of Health (NIH) – the largest medical research funding agency in the country (and in the world) – was ~$32.3 billion. Out of this general budget, in 2016, the National Institute on Aging (NIA) received about $1.6 billion (~5% of the NIH budget) and about the same in 2017.
According to the NIA budget specifications, “The FY 2017 President’s Budget request is $1,598.246 million, the same as for the FY 2016 Enacted Level.” Within the National Institute of Aging, the program “Biology of Aging” doing fundamental research of mechanisms of aging and intervention into aging processes underlying aging-related diseases, received in 2016 the budget of ~$184 million (~11.5% of the NIA, and 0.57% of the NIH budget). For 2017 “The FY 2017 President’s Budget request is $183.174 million, a decrease of $0.736 million or 0.4 percent compared to the FY 2016 Enacted level.”
Radical cuts are apparently expected in 2018: the overall NIH budget is expected to decrease to $26.9B in 2018 from $32.6B annualized budget in 2017 ($5.7B or ~17.5% reduction). The NIA expects a similar proportional reduction from $1,598.246 in 2017 to $1,303.541 in 2018 (~18% decrease). The cut appears to be even more drastic, if compared to the Fiscal Year 2017 Congressional Continuing Resolution (CR) Level: “The FY 2018 President’s Budget request is $1,303.541 million which is $745.069 million below the FY 2017 Annualized CR Level. These reductions are distributed across all programmatic areas and basic, epidemiology, or clinical research” – i.e. ~36% (over one third) reduction. For 2018, allocations for specific NIA programs were not shown in the open NIA budget presentation.
(US Department of Health and Human Services, National Institutes of Health, National Institute on Aging, “Budget & Testimony,” accessed June 2017, https://www.nia.nih.gov/about/budget; https://www.nia.nih.gov/sites/default/files/fy2018-budget-national-institute-on-aging.pdf; https://www.nia.nih.gov/sites/default/files/nia-fy2017-budget-2.pdf;
US Department of Health and Human Services, National Institutes of Health, NIH Office of Budget, “History,” accessed June 2017, https://officeofbudget.od.nih.gov/history.html; https://officeofbudget.od.nih.gov/pdfs/FY16/Approp%20History%20by%20IC%20FY%202000%20-%20FY%202016.pdf ; https://www.nih.gov/about-nih/what-we-do/budget.)
For the European Union, though the health expenditures are lower than for the US (€1723 bln or $1940 bln total, and $2,900 per capita as of 2014), the expenditures on biomedical research, and aging research in particular, appear to be lower as well, in both absolute and relative terms.
(Eurostat, “Healthcare Expenditure Statistics,” accessed, June 2017, http://ec.europa.eu/eurostat/statistics-explained/index.php/Healthcare_expenditure_statistics.)
Thus, in the EU, in May 2014, the Council of the European Union adopted a €22 billion Innovation Investment Package – for 7 years. It included a program to address the aging challenge in Europe, namely the renewed Active Assisted Joint Programme (AAL JP2). The AAL JP2 Programme received €175 million from the European Commission under the new Horizon 2020 (H2020) research framework programme, €350 million from industrial partners and at least €175 million from Member States: altogether more than €700 million for 7 years. Yet, notably, the emphasis of this investment package is to “to help Europe address the challenges and opportunities of the rapidly ageing population by supporting industry, and in particular SMEs [small and medium enterprises], to bring innovative digital products and services for ageing well to the European market” rather than developing and applying therapeutic solutions for aging-related ill health. That is, annually, ~€100 mln ($112 mln) a year would be expended on the Active Assisted Joint Programme (AAL JP2) which is about 3.1% of the Innovation Investment Package of €3.3 bln ($3.71 bln) yearly. Yet, even within the program, the part of actual biomedical research of aging is rather imperceptible.
(European Commission, Digital Single Market, “€700 million to meet European ageing population’s needs,” Projects News and Results, 06/05/2014, https://ec.europa.eu/digital-single-market/news/%E2%82%AC700-million-meet-european-ageing-population%E2%80%99s-needs.)
This relative neglect of biomedical aging R&D may be explained by the common perception that assistive technologies, “digital products and services for ageing well,” may be easier to “bring to the market” than biomedical technologies and therapies that yet require long, costly and careful investigation. The commercial rationale for valorizing ready or nearly ready products is quire clear, but the critical need to research and develop effective therapies for the aged should be clear as well. Unfortunately, this need does not appear to be strongly realized within the EU research programs.
Thus, within the main current European R&D funding framework – the EU Framework Programme for Research and Innovation – Horizon 2020, the challenge on “Health, Demographic Change and Wellbeing” places a great emphasis on improving health of the aging European population. Yet, the portion of this challenge, among all the seven societal challenges of the Horizon 2020 funding program, is not very large. The Horizon 2020 program makes available for EU research and innovation nearly €80 billion (~$90 billion) of funding over 7 years (2014 to 2020), or about €11.4 Billion ($12.8 billion) yearly. During the first four years of Horizon 2020 (Work Programmes for 2014/15 and 2016/2017), the EU invested more than €2 billion in the “Health, Demographic Change and Wellbeing” Challenge, in calls for proposals or actions. That is about €500 mln ($563 mln) yearly, or €3.5 billion for the 7 years – about 4.4% of the entire Horizon 2020 budget. The portion dedicated to actual biomedical research aimed to provide internal health benefits for the elderly, and not just seeking to develop assistive technologies or information and communication technologies (ICT) for them, is smaller still. And the proportion of therapeutic research of aging processes appears to be virtually imperceptible.
It appears there are few programs within the “Health, demographic change and wellbeing” challenge that could be related, even indirectly, to biomedical therapeutic research of aging. These include the research and innovation actions “SC1-PM-09-2016: New therapies for chronic diseases” with the budget of €60 mln for 2016, and “SC1-PM-11-2016-2017: Clinical research on regenerative medicine” with the budget of €30 mln for 2016. Together these two actions comprise €90 mln ($101 mln) for the year 2016, or ~18% of the ~€510 mln total 2016 budget for the “Health, demographic change and wellbeing” challenge, or about 0.78% of the yearly Horizon 2020 budget.
Some other programs in this challenge could also be related to biomedical aging research, but only very indirectly.
Interestingly enough, within this challenge, the programs under the heading “Active ageing and self-management of health” such as the action “SC1-PM-12-2016: PCP [pre-commercial procurement] – eHealth innovation in empowering the patient” and “SC1-PM-13-2016: PPI [public procurement of innovative solutions] for deployment and scaling up of ICT solutions for active and healthy ageing,” as well as “SC1-PM-14-2016: EU-Japan cooperation on Novel Robotics based solutions for active and healthy ageing at home or in care facilities” and “SC1-PM-15-2017: Personalised coaching for well-being and care of people as they age” – altogether receiving ~€40 mln for 2016 – do not seem to be interested in therapeutic research of aging at all, but only in developing electronic devices and information services for the elderly. This emphasis is understandable, insofar as such electronic and software products could be brought to the market quickly and can provide immediate assistive services for the elderly. However, it must be emphasized that such devices and services provide no internal health benefits for the elderly that are urgently desired and needed. Nowhere does the challenge seem to mention the need for biomedical research of the aging process directly, to enable such health benefits.
(HORIZON 2020, The EU Framework Programme for Research and Innovation, “Health, Demographic Change and Wellbeing,” accessed June 2017, http://ec.europa.eu/programmes/horizon2020/en/h2020-section/health-demographic-change-and-wellbeing; https://ec.europa.eu/programmes/horizon2020/en/h2020-section/societal-challenges;
Horizon2020, The EU Framework Programme for Research and Innovation, “What is Horizon 2020,” accessed June 2017, https://ec.europa.eu/programmes/horizon2020/en/what-horizon-2020;
Horizon 2020, Work Programme 2016 – 2017, “8. Health, demographic change and well-being,” http://ec.europa.eu/research/participants/data/ref/h2020/wp/2016_2017/main/h2020-wp1617-health_en.pdf.)
It should be additionally noted that the expenditures on aging-related biomedical research (as we have seen roughly in the range of a few hundred millions of dollars per year at most for the major superpowers) are really tiny as compared to general R&D expenditures. Thus, as of 2014, for the US the total R&D expenditures were estimated to be $485 bln or 2.78% of the country’s Gross Domestic Product (GDP), and for the EU, for 2014, the estimates were respectively €283 bln (~$320 bln) or 2.03% of the EU GDP.
The proportion should hopefully change in favor of enhancing the state budget for biomedical aging research and development.
It should be further added that the main part of the general estimated R&D expenditures is the industrial and commercial R&D, seemingly without direct governmental involvement and budget support. Yet, arguably, governmental recognition and raising public awareness for the importance of the problems of aging and the R&D dedicated to address these problems, and the establishment of relevant R&D programs with governmental support, can encourage public demand and consequently the commercial R&D as well.
(Industrial Research Institute, “2016 GLOBAL R&D,” Winter 2016, http://www.iriweb.org/; https://www.iriweb.org/sites/default/files/2016GlobalR%26DFundingForecast_2.pdf;
Eurostat – News Release, “R&D expenditure in the EU stable at slightly over 2% of GDP in 2014. Almost two thirds spent in the business sector,” 30 November 2015, http://ec.europa.eu/eurostat/documents/2995521/7092226/9-30112015-AP-EN.pdf/29eeaa3d-29c8-496d-9302-77056be6d586;
Eurostat, “R&D Expenditure,” accessed June 2017, http://ec.europa.eu/eurostat/statistics-explained/index.php/R_%26_D_expenditure.)
[5]. Alex Zhavoronkov, Bhupinder Bhullar, “Classifying aging as a disease in the context of ICD-11,” Frontiers in Genetics, 6, 326, 2015, http://journal.frontiersin.org/article/10.3389/fgene.2015.00326/full;
Sven Bulterijs, Raphaella S. Hull, Victor C.E. Björk, Avi G. Roy, “It is time to classify biological aging as a disease,” Frontiers in Genetics, 6, 205, 2015, http://journal.frontiersin.org/article/10.3389/fgene.2015.00205/full;
Ilia Stambler, “Has aging ever been considered healthy?” Frontiers in Genetics, 6, 202, 2015, http://journal.frontiersin.org/article/10.3389/fgene.2015.00202/full.
[6] Ilia Stambler, “Recognizing degenerative aging as a treatable medical condition: methodology and policy,” Aging and Disease, 8(5), 2017, http://www.aginganddisease.org/EN/10.14336/AD.2017.0130.
[7]. World Health Organization, International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10)-WHO Version for 2016, Geneva, 2016, http://apps.who.int/classifications/icd10/browse/2016/en#R54;
2017 ICD-10-CM, Diagnosis Code R54, Age-related physical debility, 2017, http://www.icd10data.com/ICD10CM/Codes/R00-R99/R50-R69/R54-/R54;
World Health Organization, ICD-11 Beta Draft (Joint Linearization for Mortality and Morbidity Statistics), MJ35 Old Age, accessed June 2017, http://apps.who.int/classifications/icd11/browse/l-m/en#/http://id.who.int/icd/entity/835503193.
[8] World Health Organization, Global Strategy and Action Plan on Ageing and Health (GSAP) – 2016-2020, November 2015, http://www.who.int/ageing/global-strategy/en/; http://apps.who.int/gb/ebwha/pdf_files/WHA69/A69_17-en.pdf?ua=1.
[9]. European Medicines Agency, Medicines for older people, London, accessed June 2017, http://www.ema.europa.eu/ema/index.jsp?curl=pages/special_topics/general/general_content_000249.jsp.
Some of the major relevant EMA documents on geriatric evaluation and treatment that are available from this site, include:
European Medicines Agency, EMA geriatric medicines strategy, EMA/CHMP/137793/2011;
European Medicines Agency, EMA geriatric medicines strategy: Report analysis on product information, EMA/352652/2013;
European Medicines Agency, Concept paper on the need for a reflection paper on quality aspects of medicines for older people, EMA/165974/2013;
European Medicines Agency, Proposal for the development of a points to consider for baseline characterisation of frailty status, EMA/335158/2013.
See also:
Cesari M., Fielding R., Bénichou O., Bernabei R., Bhasin S., Guralnik J.M., et al., “Pharmacological interventions in frailty and sarcopenia: Report by the International Conference on Frailty and Sarcopenia Task Force,” The Journal of Frailty & Aging, 4(3), 114-120, 2015, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4563815/.
[10]. US Department of Health and Human Services. Food and Drug Administration (FDA), Guidance for industry. E7 studies in support of special populations: Geriatrics. Questions and answers, Food and Drug Administration, Silver Spring, Maryland, 2012, http://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm189544.pdf;
US Department of Health and Human Services. Food and Drug Administration (FDA), ICH Guidance Documents, accessed June 2017, http://www.fda.gov/ScienceResearch/SpecialTopics/RunningClinicalTrials/GuidancesInformationSheetsandNotices/ucm219488.htm.
[11]Healthspan Campaign, “Dr. Nir Barzilai on the TAME Study,” April 28, 2015, http://www.healthspancampaign.org/2015/04/28/dr-nir-barzilai-on-the-tame-study/;
Stephen S. Hall, “A trial for the ages,” Science, 349(6254), 1275-1278, 2015, http://www.sciencemag.org/news/2015/09/feature-man-who-wants-beat-back-aging;
John C. Newman, Sofiya Milman, Shahrukh K. Hashmi, Steve N. Austad, James L. Kirkland, Jeffrey B. Halter, Nir Barzilai, “Strategies and Challenges in Clinical Trials Targeting Human Aging,” Journal of Gerontology: Biological Sciences, 71(11), 1424-1434, 2016, https://academic.oup.com/biomedgerontology/article/71/11/1424/2577175/Strategies-and-Challenges-in-Clinical-Trials.
[12] Madhukar Pai, “Essential medicines require essential diagnostics,” Huffington Post, June 12, 2017, http://www.huffingtonpost.ca/dr-madhukar-pai/essential-medicines-diagnostics_b_17047540.html;
WHO Technical Report Series, Report of the WHO Expert Committee on Selection and Use of Essential Medicines, 2017 (including the 20th WHO Model List of Essential Medicines and the 6th WHO Model List of Essential Medicines for Children), 2017, http://www.who.int/medicines/publications/essentialmedicines/EML_2017_EC21_Unedited_Full_Report.pdf?ua=1.
[13] Robert Preidt, “FDA Approves Flu Shot to Boost Immune Response. Vaccine can be used in seniors, who are often hit hardest by illness,” WebMD News from HealthDay, November 25, 2015, http://www.webmd.com/cold-and-flu/news/20151125/fda-approves-first-flu-shot-with-added-ingredient-to-boost-immune-response.
[14]. Natalia Olchanski, Yue Zhong, Joshua T. Cohen, Cayla Saret, Mohan Bala, Peter J. Neumann, “The peculiar economics of life-extending therapies: a review of costing methods in health economic evaluations in oncology,” Expert Review of Pharmacoeconomics & Outcomes Research, 15(6), 931-940, 2015.
[15]. James L. Bernat, “Medical futility: definition, determination, and disputes in critical care,” Neurocritical Care, 2(2), 198-205, 2005.
[16] Alan A. Cohen, “Complex systems dynamics in aging: new evidence, continuing questions,” Biogerontology, 17(1), 205-220, 2016, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4723638/;
David Blokh, Ilia Stambler, “The application of information theory for the research of aging and aging-related diseases,” Progress in Neurobiology, S0301-0082(15)30059-9, 2016, doi: http://dx.doi.org/10.1016/j.pneurobio.2016.03.005;
Alexey Moskalev, Elizaveta Chernyagina, Vasily Tsvetkov, Alexander Fedintsev, Mikhail Shaposhnikov, Vyacheslav Krut’ko, Alex Zhavoronkov, Brian K. Kennedy, “Developing criteria for evaluation of geroprotectors as a key stage toward translation to the clinic,” Aging Cell, 15(3), 407-415, 2016, http://onlinelibrary.wiley.com/wol1/doi/10.1111/acel.12463/full;
Alexey Moskalev, Elizaveta Chernyagina, Anna Kudryavtseva, Mikhail Shaposhnikov, “Geroprotectors: a unified concept and screening approaches,” Aging and Disease, 8(3), 354-363, 2017, http://www.aginganddisease.org/EN/10.14336/AD.2016.1022;
Vasilij N. Novoseltsev, Janna Novoseltseva, Anatoli I. Yashin, “A homeostatic model of oxidative damage explains paradoxes observed in earlier aging experiments: a fusion and extension of older theories of aging,” Biogerontology, 2(2), 127-138, 2001, https://link.springer.com/article/10.1023/A:1011511100472.
[17]. Yu Luo, Garud Iyengar, Venkat Venkatasubramanian, “Soft regulation with crowd recommendation: coordinating self-interested agents in sociotechnical systems under imperfect information,” PLoS One, 11(3), e0150343, 2016.
[18]. Fujita Y., Kawamoto A., “Regenerative medicine legislation in Japan for fast provision of cell therapy products,” Clinical Pharmacology & Therapeutics, 99(1), 26-29, 2016.
[19]. R. Alta Charo, “On the Road (to a Cure?) – Stem-Cell Tourism and Lessons for Gene Editing,” New England Journal of Medicine, 374(10), 901-903, 2016, http://www.nejm.org/doi/full/10.1056/NEJMp1600891#t=article.
[20]. Jeremy A. Greene, “Do-It-Yourself Medical Devices – Technology and Empowerment in American Health Care,” New England Journal of Medicine, 374(4), 305-308, 2016, http://www.nejm.org/doi/full/10.1056/NEJMp1511363#t=article.
[21]. United States Government Accountability Office, New Drug Development: Science, Business, Regulatory and Intellectual Property Issues Cited as Hampering Drug Development Efforts, 2006, http://www.gao.gov/products/GAO-07-49;
Steve Morgan, Paul Grootendorst, Joel Lexchin, Colleen Cunningham, Devon Greyson, “The cost of drug development: a systematic review,” Health Policy, 100(1), 4-17, 2011, http://www.sciencedirect.com/science/article/pii/S0168851010003659.
[22] John Harris, “Immortal Ethics,” presented at the International Association of Biogerontologists (IABG) 10th Annual Conference “Strategies for Engineered Negligible Senescence,” Queens College, Cambridge, UK, September 17-24, 2003, reprinted in: Aubrey de Grey (Ed.), Strategies for Engineered Negligible Senescence: Why Genuine Control of Aging May Be Foreseeable, Annals of the New York Academy of Sciences, 1019, 527-534, June 2004.
[23] World Health Organization, Global Strategy and Action Plan on Ageing and Health (GSAP) – 2016-2020, November 2015, “Plan of Action, 2016-2020, 3.3. Member States,” http://www.who.int/ageing/global-strategy/en/; http://apps.who.int/gb/ebwha/pdf_files/WHA69/A69_17-en.pdf?ua=1.
[24] US National Institute on Aging (NIA), “Featured Health Topic: Healthy Aging/Longevity,” accessed June 2017, https://www.nia.nih.gov/health/featured/healthy-aging-longevity.
[25]. Aftab Ahmad, Shoji Komai, “Geriatrics and gerontology: neglected areas of research in most developing countries,” Journal of the American Geriatrics Society, 63(6), 1283-1284, 2015, doi: http://dx.doi.org/10.1111/jgs.13521.
 Happy Longevity Day! – October 1 – The Beginning of the “Longevity Month” campaign of October to promote biomedical research of aging to improve Healthy Longevity for the global population! (Following the UN International Day of Older Persons)
Happy Longevity Day! – October 1 – The Beginning of the “Longevity Month” campaign of October to promote biomedical research of aging to improve Healthy Longevity for the global population! (Following the UN International Day of Older Persons)